What is a shoulder replacement?
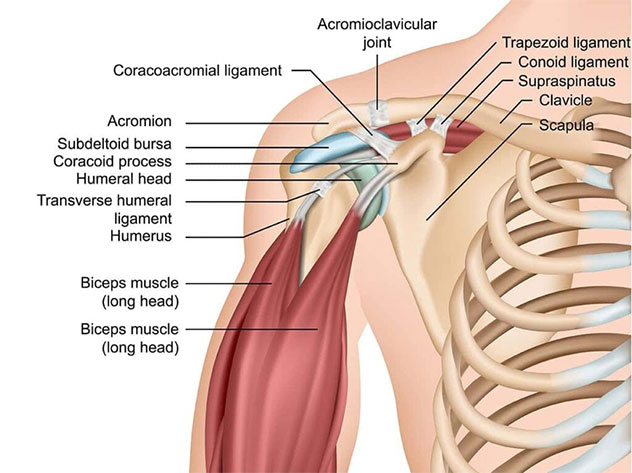
A shoulder replacement is also known as ‘shoulder arthroplasty’, and is an operation that replaces the damaged joint with an implant (also known as a ‘prosthesis’). The types of implants used can either replace part or all of the shoulder joint. A total shoulder replacement involves placing an implant on both the socket side (glenoid) and the ball side (head of the humerus). Furthermore, the geometry of the implant used can either be ‘anatomic’ which aims to closely replicate the natural anatomy of the shoulder, or ‘reversed’ which aims to compensate for weak or damaged muscles around the shoulder.
What conditions is a total shoulder replacement used for?
A total shoulder replacement may be a surgical option for several conditions affecting the shoulder. These include:
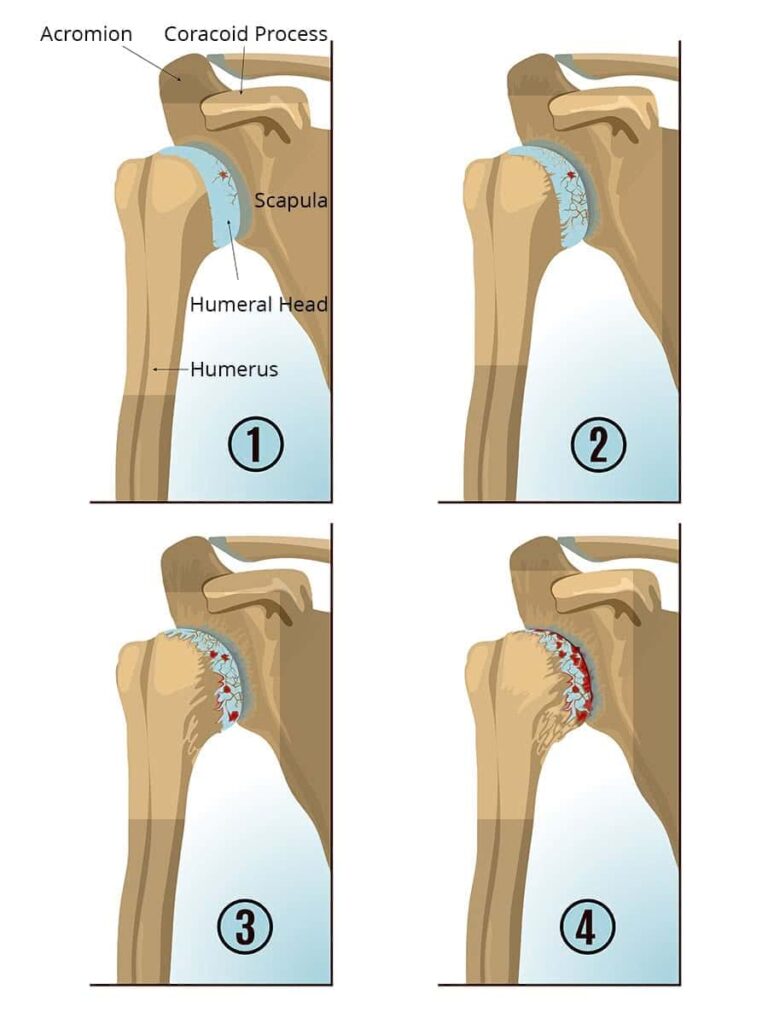
- Osteoarthritis – a degenerative condition leading to damage of the joint cartilage of the shoulder.
- Rheumatoid arthritis – an autoimmune condition which leads to inflammation of the lining (synovium) of the joint, which eventually leads to destruction of the joint cartilage.
- Post traumatic arthritis – damage to the joint cartilage as a result of a fracture involving the joint surface, or due to recurrent dislocations.
- Rotator cuff arthropathy – as a result of long-standing damage to the rotator cuff tendons supporting the shoulder, altered biomechanics leads to eventual joint surface disease.
- Avascular necrosis – loss of blood supply to the bone of the humeral head leads to collapse and destruction of the joint.
- Fracture – a bad broken bone involving the upper part of the humerus may not be reconstructable and joint replacement may be a more reliable solution.
Is a shoulder replacement the right option for you?
The diseased and damaged shoulder can lead to many problems. The main symptoms are pain and stiffness. When these symptoms begin to impact on quality of life and function in daily life, then it may be time to consider a shoulder replacement.
Evaluation for a shoulder replacement
Prior to consideration of a shoulder replacement for arthritis, the non-operative options should be trialled. These will include simple analgesia and anti-inflammatory medication, trial of corticosteroid injections, and physiotherapy to improve function. Should these non-operative measures be unsuccessful, then you will be evaluated to see if you are a candidate for shoulder replacement surgery.
What’s involved in a shoulder replacement?
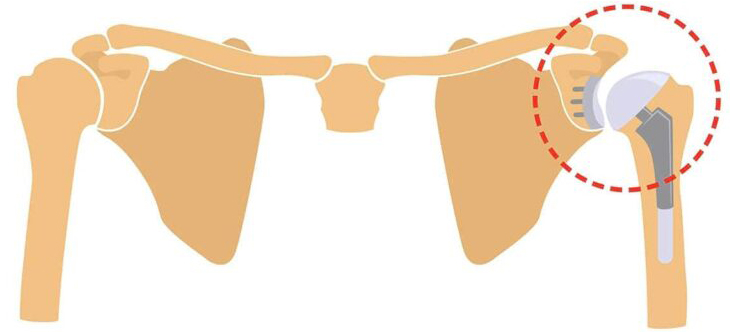
An anatomic or ‘conventional’ total shoulder replacement
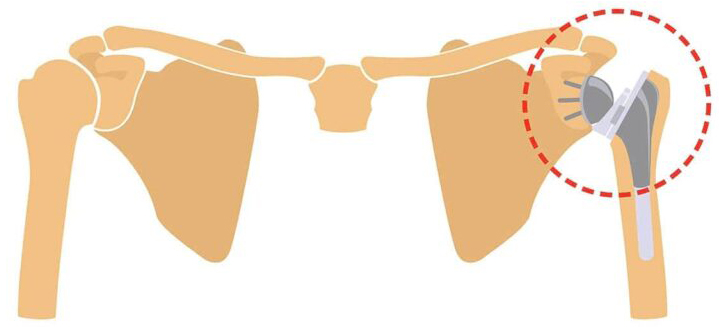
A ‘reverse’ total shoulder replacement
The skin incision for a shoulder replacement is made over the front and outer aspect of the shoulder. It is 10-12cm in length. The tendons of the rotator cuff muscles are inspected and the subscapularis muscle is lifted from the bone in order to give access to the joint. This muscle is repaired at the end of the procedure.
The joint surfaces are then inspected and removed. The implants are then sized, trialled and implanted. In an ‘anatomic’ shoulder replacement, the cup of the implant is inserted on the cup of the shoulder blade (glenoid), and the ball of the implant is inserted into the arm bone (humerus). In a ‘reverse’ shoulder replacement, the geometry is reversed. That is, the cup of the implant is inserted on the humerus, and the ball of the implant is inserted on the glenoid. This design helps to compensate for a weak or torn rotator cuff.
Following insertion of the implants, the shoulder is tested for range of motion and stability. The subscapularis muscle is repaired and the incision is closed using absorbable stitches.
Risks

As with any surgical procedure, there is a small risk of:
-
- Infection
- Wound healing problems
- Cardiovascular risks – stroke, heart attack, blood clots
- Bleeding
- Swelling of the operated limb – generally subsides within weeks to months.
- Pain – discomfort is expected after an operation, however pain medications are used in a routine manner to relieve this post-operative discomfort
Specific risks of a total shoulder replacement are:
-
- Damage to nerves around the shoulder
- Stiffness or ‘frozen shoulder’
- Failure of tendon healing
- Loosening of the implant
- Infection of the implant
- Fracture around the implant
- Revision surgery
What happens after the surgery?

Postoperative instructions and follow up
Immediate post-op
After your operation you will be taken to the recovery room of the hospital, and allowed to have something to drink. When the team is happy the anaesthetic has worn off, you will be transferred to the day surgery area or to your inpatient room depending on whether you will be staying overnight. A sling / shoulder immobiliser would have been placed on your arm in the operating room, and should keep your arm comfortable and safe. If a nerve block has been performed by our anaesthetist, then your arm should feel comfortable but numb for up to 24-36 hours after the operation. When pins-and-needles are felt in the hand and arm then the block is starting to wear off, and your nursing staff will commence pain medication to keep you comfortable.
Discharge from hospital
On discharge from hospital you will be given:
- Physiotherapy – instructions on exercises that should commence for the shoulder, elbow and wrist.
- Sling – instructions on the use of your sling, including whether it is allowed to be removed.
- Dressings – please keep dressings dry and do not remove them.
- Follow up appointment time
Follow up
A follow up appointment will have been made for you after the operation. This will typically be an appointment around the 2-3 weeks after the surgery. If you have any concerns before this appointment, call Dr Yu’s clinic on (08) 7099 0188 to speak with us.
My goals as a surgeon are to relieve your pain, restore your function, and return you back to doing what you love.
– Dr Raymond Yu
- Adelaide Orthopaedic Surgeon
- Adelaide Shoulder Surgeon
About
Dr Raymond Yu
Dr Raymond Yu is an Adelaide Orthopaedic Surgeon with post-Fellowship expertise in Shoulder and Elbow Surgery.
He specialises in orthopaedic surgery of the Shoulder and Upper Limb with a focus on modern keyhole and minimally-invasive techniques.
Dr Yu has a special passion for:
- Rotator cuff repair surgery
- Shoulder replacement surgery
- Shoulder stabilisation surgery
Dr Yu practices at